Trabeculectomy with Mitomycin (anti-metabolite)
The trabeculectomy is the most common incisional glaucoma surgeon that Dr. Schertzer performs. By bypassing the normal drainage channels for the fluid within the eye with a partial thickness trap-door in the sclera (white of the eye) underneath the upper-lid, the intraocular pressure is reduced. After the full 6-8 week recovery period, there will be a slightly raised area on the surface of the eye, called a ‘bleb,’ through which the diverted fluid evaporates and gets re-absorbed by blood vessels in the overlying vascular layer covering the sclera (the conjunctiva.)
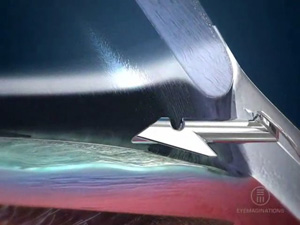
 The Optonol ExPress Mini-Shunt
The Optonol ExPress Mini-Shunt
In 2008, the ExPress mini-shunt was approved for use in Canada. With long-term results similar to those obtained with the trabeculectomy, use of this surgical steel tube to maintain the steady flow of aqueous humour under the scleral flap to form the bleb has a more predictable early post-operative course than the standard trabeculectomy. Unfortunately, although the surgery is covered by MSP, our hospital’s operating room budget does not cover the cost of this implant. This procedure, as of 2020, is no longer in common use.
 The Ahmed Glaucoma Valve
The Ahmed Glaucoma Valve
When a trabeculectomy fails or is likely to fail due to previous eye surgery, a glaucoma drainage device is indicated. Dr. Schertzer tends to prefer the Ahmed Glaucoma Valve for most of these situations, either the single-plated FP7 model or the double-plated FX1 model (when an extremely low pressure is needed.) On occasion, the Baerveldt glaucoma drainage device will be used but tends to have a less predictable post-operative course with similar long-term results.
Cataract Surgery in glaucoma patients
Most glaucoma patients can safely have cataract surgery when the time comes performed by their primary ophthalmologist. If you do not already have a cataract surgeon as your primary ophthalmologist, and your cataracts advance to the point where you are beginning to have difficulty seeing well enough to perform your daily activities such as reading, working on the computer, watching TV, or driving, then Dr. Schertzer is qualified to perform your cataract surgery. He is quite used to some of the additional challenges that can occur in patients who have had prior glaucoma surgery and will follow you closely after the surgery to make sure your glaucoma remains in good control following the cataract surgery.
Combined Glaucoma and Cataract Surgery
As glaucoma can result in permanent damage if not treated in a timely manner, whereas the vision lost from cataracts returns following cataract surgery even if surgery is delayed, Dr. Schertzer usually recommends that glaucoma surgery be performed first in patients who have glaucoma that requires surgical intervention as well as visually significant cataracts. In addition, Dr. Schertzer feels that the glaucoma surgery results in a lower post-operative eye pressure value when performed on its own, instead of being combined with cataract surgery. That being said, there are times when the two surgeries may be performed at the same time. One such situation is if the glaucoma is stable on current medical treatment but to do so is requiring the use of multiple glaucoma medications which are having too many side effects. Therefore, combining the cataract surgery with the glaucoma surgery can results in the need for fewer or even no glaucoma medications. For other patients, it is just not practical to be subjected to two surgeries when both are going to be needed fairly soon in order to achieve useful vision. Therefore, sometimes glaucoma and cataract surgery can be combined.
Contact Transcleral Laser Cycloablation (CTLC or diode laser ablation)
Although technically this is not ‘incisional’ surgery as no sharp instruments are used to make any incision into the eye, this procedure is listed in the surgery category as it is the treatment of choice when it is too late for any of the above surgeries to be of help. The ciliary body is responsible for the production of aqueous humour, the fluid that circulates within the eye. Most treatment methods for glaucoma either decrease the production of this fluid or improve its outflow through the trabecular meshwork and the uveoscleral routes. This procedure focuses laser energy on the ciliary body through the sclera and conjunctiva on the outside of the eye by touching a probe that is the size of a pen onto the surface of the eye, just beyond the edge of the cornea. We perform this procedure in a treatment room on the ground floor of the VHHSC/UBC Eye Care Centre that is adjacent to our building. This is one of the few procedures that cannot be performed with just topical anaesthesia; we need to perform a regional block by injecting a local anaesthetic agent around your eye. After the treatment, you will be prescribed anti-inflammatory drops to use frequently over a number of weeks and will usually be seen back for your first follow-up visit one week later.
View Video
© Dr. Robert Schertzer Inc. 2020

 The Optonol ExPress Mini-Shunt
The Optonol ExPress Mini-Shunt The Ahmed Glaucoma Valve
The Ahmed Glaucoma Valve