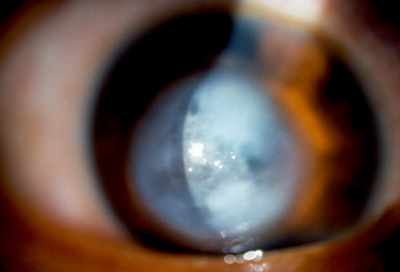
Keratoconus is an uncommon condition in which the dome-shaped cornea (the clear front window of the eye) becomes thin and develops a cone-like bulge. As the condition progresses, the shape of the cornea is altered, distorting your vision. Usually, keratoconus affects both eyes, although symptoms and progression in each eye may differ.

Early symptoms include mild blurring of vision, increased sensitivity to light and glare, and mild eye irritation. The rate of progression varies. Keratoconus usually begins in the teenage years. It may progress slowly for 10 to 20 years and then suddenly stop. As it progresses, the most common symptoms are increased blurring, increased nearsightedness or astigmatism, inability to wear contact lenses, and frequent eyeglass prescription changes.
The causes of keratoconus are not known. Since an estimated 10% of people with keratoconus have a family member with the condition, some researchers believe genetics may play a role.
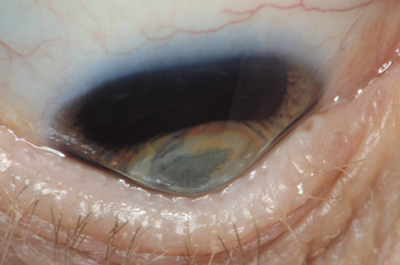
Keratoconus is usually corrected with eyeglasses. However, as the condition progresses, rigid contact lenses may be needed so that vision is improved. If vision is greatly affected (such as following a sudden swelling of the cornea in the form of ‘hydrops’ as pictured below), a corneal transplant may be recommended. While this procedure will relieve the symptoms of keratoconus, it will not cure it completely. Nonetheless, corneal transplants offer the best prognosis for clear vision.
A new technique recently has been evaluated to treat progressive keratoconus. This technique involves placing crescent-shaped acrylic inserts in the midperiphery of the cornea. This has been shown to be effective in some patients. You should discuss this technology with your ophthalmologist (Eye M.D.).
(c) 2009 Robert M. Schertzer, MD, MEd, FRCSC adapted from 2007 The American Academy of Ophthalmology
