If your cornea is severely damaged or diseased, you might require a corneal transplant to improve your vision.
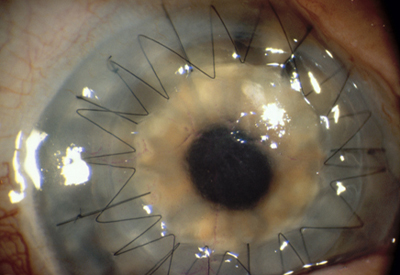
One type of corneal transplant, called a penetrating keratoplasty (PKP), replaces your central corneal tissue with donor tissue. (See photo below.) The procedure usually takes about an hour under regional or general anesthesia, and you can go home the same day following surgery. After corneal transplant surgery, you will wear a plastic shield or eyeglasses to protect your eye, and you will use eyedrops to prevent infection and rejection of the donor tissue. Your ophthalmologist (Eye M.D.) will monitor your progress closely after your surgery to ensure the best possible visual outcome and to control minor discomfort associated with the surgery and healing process. Vision usually returns gradually over the next few months or up to a year. It is important to inform your ophthalmologist if you have pain, irritation, or redness of the eye following PKP, as this could be the earliest sign of infection or rejection, and early treatment of these conditions is critical to the viability of your graft.
Another corneal transplant procedure is called a lamellar keratoplasty. This is an advanced technique that replaces only the superficial layers of your cornea using donor tissue, leaving the lower layers of tissue intact. DSEK – Descemet’s Stripping Endothelial Keratoplasty (see video below) leaves the superficial layer of the cornea intact but replaces the posterior layers of the cornea and is increasing in popularity. Although these are more technically challenging procedure than penetrating keratoplasty, it may reduce the risk that your body will reject the donor tissue and is a good option for some patients. Currently, Penetrating Keratoplasty remains the standard of care for most patients in Canada.
(c) 2009 Robert M Schertzer MD, MEd, FRCSC based on 2007 The American Academy of Ophthalmology