Pigmentary dispersion syndrome (PDS)
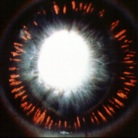
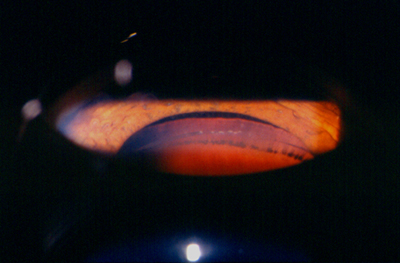
Pigment Dispersion Syndrome is a condition in which increased amounts of pigment circulate within the front portion of the eye. This often results in the deposition of pigment on the back of the cornea, thinning of the iris, the creation of characteristic ‘Transillumination Defects,’ and the clogging of the ocular drainage system with pigment. A pathognomonic finding is the deposition of pigment behind the crystalline lens, known as Scheie’s Line.
Pigmentary Glaucoma
This dispersed pigment can block the drainage channel enough to cause an increase in intraocular pressure (IOP). If the eye’s drainage system clears the pigment without damaging the drainage channels, then the eye pressure does not remain elevated. However, should the trabecular meshwork be damaged by the body’s reaction to the pigment, the pressure will rise, and glaucoma can result.
In cases of pigmentary glaucoma, the IOP is often very high, reaching levels above 40 mm Hg. Pigmentary dispersion leads to pigmentary glaucoma in 15% to 50% of patients. It is more common in males and often appears in people under 50 years of age.
Treatment
Treatment is the same as for other forms of open-angle glaucoma, including medications, laser therapy, or surgery. With adequate treatment, the prognosis for pigmentary glaucoma is good.
© 2025, 2020, 2015, 2009 Dr. Robert Schertzer Inc. based on 2007 The American Academy of Ophthalmology
